HAWZEN, Tigray Region – Nine-months pregnant with her first child, Tigist Gebrerefael, 23, did not want to experience the agony other women in her rural enclave had endured during childbirth. “I have seen my sister and many other pregnant women suffering or dying due to the lack of maternal health services and medication during the conflict,” she said.
Pregnancy and childbirth pose some the biggest risks to a woman's life and health, because at any stage, things can go wrong. She could die from haemorrhage, or excessive bleeding, one of the leading causes of maternal death worldwide. Or she may endure an obstructed labour causing a fistula or hole between the birth canal and bladder or rectum, leaving her childless and leaking urine or faeces. If she has high blood pressure during pregnancy, she could suffer a seizure.
For all of these conditions, timely medical intervention is key. Yet his was not possible for Ms. Gebrerefael.
“The health centre at my village was destroyed during the conflict,” she said.
We are thankful that now we can travel freely to reach health services.
In November last year, a cessation of hostilities agreement was signed between the Ethiopian government and the Tigray People's Liberation Front. The peace accord means that pregnant women are once more able to move around once more to get the medical attention they need.
“We are thankful that now we can travel freely to reach health services,” she said.

As her delivery date approached, Ms. Gebrerefael wanted to be safe and stay close to medical services. She had heard about Maedot’s Maternity Waiting Home at Megab Health Centre in Hawzen, and decided to await her time there. But her journey involved an epic three-hour trek through mountainous terrain from Koraro, the rural area where she lives with her husband and family.
“I was carried on a wooden stretcher by members of my community because there is no transport,” she said. Thankfully, the trip went without incident, and Ms. Gebrerefael is able to rest in comfort while she awaits her special day.
Staying here gives me confidence with my pregnancy and childbirth.
“Pregnant women can stay for the last weeks of their pregnancy, while receiving services like antenatal care, ultrasound checks, follow-ups on vital signs or birth preparedness information. In case of severe medical conditions, they are referred to specialized services,” said Dr. Alem, a medical doctor and sexual and reproductive health specialist for UNFPA in Tigray.
“Staying here gives me confidence with my pregnancy and childbirth. I can’t wait to meet my baby,” she said.
Destruction of critical health services
The two-year conflict in Tigray has left health facilities all but destroyed. Almost 80 per cent of them are non-functional1, severely compromising the delivery of lifesaving health services, including maternal and newborn care.
Like Ms. Gebrerefael, many mothers-to-be have found some solace in the peace agreement. Safety and security has improved significantly across the region, allowing mobility and access to health services. Yet health facilities remain significantly overstretched in terms of resources and staff capacity to provide comprehensive health services, compared to before the conflict.
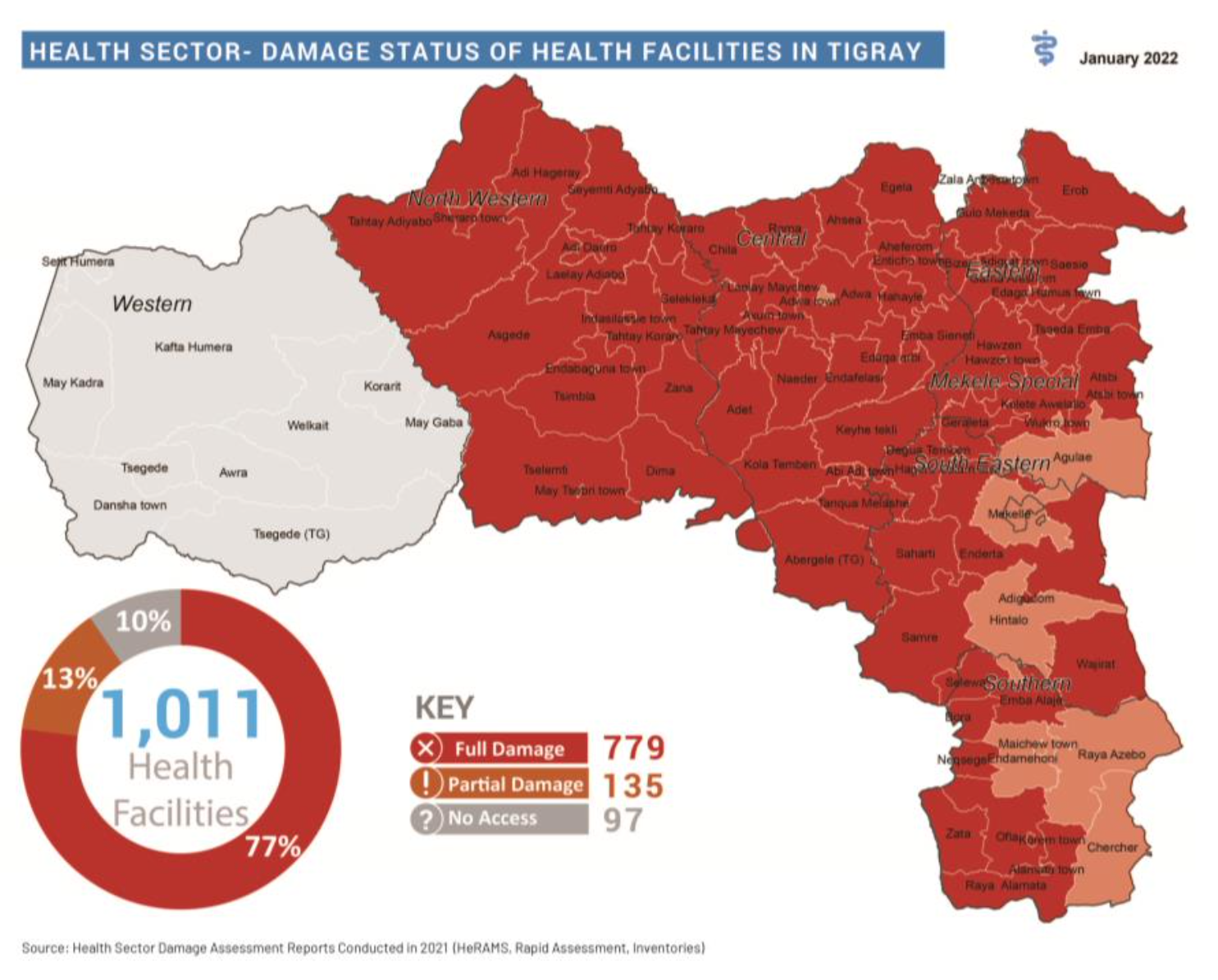
Hawzen Health Centre, for instance, is meant to serve six districts but due to the destruction of nearby health facilities, now supports nine districts. Pregnant women typically arrive on foot because the local ambulance was looted. Critical services, like the prevention of mother-to-child transmission of HIV, are not available due to the lack of treatment and medicines.
Since the onset of the conflict, the Maternal Mortality Ratio (MMR) has increased five-fold in the region, according to a study by the Regional Health Bureau and Mekelle University in May 2022. Health professionals ascribe this level to that of 22 years ago, a significant step backwards.
The provision of maternal and newborn care remains challenging due to the high number of non-functional health facilities, shortages of medical supplies, and the scarcity of ambulances and fuel for referrals.
Preventing maternal deaths
In Ethiopia, maternity waiting homes contribute an 80 per cent reduction in maternal deaths and 70 per cent in the occurrence of stillbirths, recent studies showed. These homes are one of UNFPA’s key strategies for improving access to comprehensive obstetric care for pregnant women living far from health facilities - particularly rural settings - and to prevent maternal and newborn deaths and injuries due to home deliveries.
If it was not for maternity waiting homes, we would be dealing with even higher obstetric complications, like fistula or death.
Ethiopia's maternal mortality ratio is a high 401 deaths per 100,000 live births (2017), compared to the estimated global rate of 223 maternal deaths per 100,000 live births (2020). The SDG target for maternal deaths is for a global maternal mortality ratio (MMR) of less than 70 maternal deaths per 100,000 live births by 2030.
“If it was not for maternity waiting homes, we would be dealing with even higher obstetric complications during pregnancy and childbirth, like fistula or death,” said Dr. Alem.
Recovering health systems capacity in Tigray
Last year, UNFPA reached almost 235,000 people affected by the crisis with sexual and reproductive health services, by deploying 156 midwives and 41 Mobile Health and Nutrition Teams (MHNT), to support maternal and reproductive health-care services in hard-to-reach areas countrywide. Medical supplies and equipment were distributed to more than 150 health facilities and benefitted more than 2.2 million people across nine affected regions.
In Tigray, UNFPA has reached more than 96,000 displaced women and girls with sexual and reproductive health services, through 193 midwives and health extension workers deployed to support maternity waiting homes and affected health facilities in 2023. These services are provided with the support of Canada, the Ministry of Women and Social Affairs, the World Bank, UNOPS, Irish Aid, USAID and Italy.
Furthermore, more than 237 metric tons of reproductive health kits, dignity kits, medical equipment and supplies were distributed to 34 health facilities in the region during the first quarter of 2023. These supplies will benefit more than half a million people with sexual and reproductive health and gender-based violence services.
I wish peace will remain and we are able to come back to our peasant life.
However, despite efforts to increase the coverage of maternal and reproductive health care, more support is needed to build back the health system’s capacity to respond to the needs of women in the region, like Ms. Gebrerefael.
UNFPA's humanitarian response appeal of $45 million seeks to strengthen the health system and build back capacities on maternal and reproductive health services in Tigray and other 7 crisis-affected regions, through the end of 2023. To date, 39 per cent of the humanitarian appeal remains unfunded.
For Ms. Gebrerefael, the end of conflict in the region is a blessing, particularly with her baby on the way. “I wish peace will remain and we are able to come back to our peasant life. I want my child to know no suffering,” she said.